Research Updates
AACR Annual Meeting 2024 Highlights:Extraordinary Science Across the Cancer Research Continuum
With a record number of more than 23,200 registrants, the American Association for Cancer Research® (AACR) Annual Meeting 2024 kicked off on April 7 with an Opening Ceremony that celebrated a banner year for the organization and the achievements made against cancer.
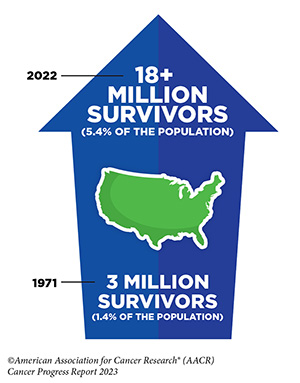 “Progress against cancer continues at a remarkable pace due to unprecedented leaps in our understanding of cancer and in cutting-edge technologies that are allowing us to target this disease with greater precision than ever before,” said Margaret Foti, PhD, MD (hc), CEO of the AACR. “Thanks to the tireless efforts of the cancer research community, the number of cancer survivors in the U.S. has now surpassed 18 million, and the cancer death rate has declined 33% over the past three decades.”
“Progress against cancer continues at a remarkable pace due to unprecedented leaps in our understanding of cancer and in cutting-edge technologies that are allowing us to target this disease with greater precision than ever before,” said Margaret Foti, PhD, MD (hc), CEO of the AACR. “Thanks to the tireless efforts of the cancer research community, the number of cancer survivors in the U.S. has now surpassed 18 million, and the cancer death rate has declined 33% over the past three decades.”

AACR President Philip D. Greenberg, MD, the Rona Jaffe Foundation endowed chair and professor and head of the program in immunology at Fred Hutchinson Cancer Research Center in Seattle, whose term as president ended on April 8, added that this year’s Annual Meeting program was designed for a unique, exciting time in cancer research.
“When we look at the intersections between basic research, preclinical science, and clinical applications—and the remarkable advances in technology that make these intersections feasible—it is clear that we come together for this Annual Meeting at a crucial moment in cancer research, a moment in which we have the potential to make quantum leaps forward in cancer etiology, prevention, diagnosis, and treatment,” Dr. Greenberg said.
Communicating great advances and the excitement they engender to the public in terms that are readily understandable is of utmost importance, especially in this time of declining trust in science.”
Philip D. Greenberg, MD
AACR President 2023-2024
|
The Opening Ceremony recognized (1) the 2024 Class of Fellows of the AACR Academy, a number of (2) recipients of this year’s scientific achievement awards, (3) the winners of the June L. Biedler Prize for Cancer Journalism, and (4) the AACR Outstanding Achievement Award for Service to Cancer Science and Medicine, which was presented to Pfizer Inc. and the company’s chairman and CEO, Albert Bourla, PhD. Last December, Pfizer announced that it will donate the rights of its royalties from the sale of the immunotherapy drug avelumab (Bavencio) in the U.S. to the AACR as an acknowledgment of the AACR’s unwavering dedication to sustained innovation in cancer research and its application to improved cancer care. |
During the Opening Ceremony, Dr. Foti acknowledged the efforts of (5) the 45 patient advocates and more than 20 advocate mentors of the AACR Scientist↔Survivor Program®. This year also marks (6) the 25th anniversary of AACR-Women in Cancer Research (WICR). Prior to WICR’s formation, only 14% of the AACR’s membership were women, including only three of the organization’s first 72 presidents. Today, women represent 45% of all AACR members and eight of the last 16 AACR presidents.
As Dr. Greenberg’s tenure as AACR president drew to a close, he wanted to ensure this year’s program set the stage for accomplishing one of his goals: providing opportunities for scientists to improve their communication skills. On April 6, he gave introductory remarks in a special session on “Strategies to Effectively Communicate Science to the Public” that featured perspectives and tips from researchers, journalists, and patient advocates on the best ways to turn scientific information into comprehensible messages for the media, policymakers, and the public.
“Communicating great advances and the excitement they engender to the public in terms that are readily understandable is of utmost importance, especially in this time of declining trust in science,” Dr. Greenberg said.
► Today, women represent 45% of all AACR members and eight of the last 16 AACR presidents.
Accelerated Aging in Younger Generations May Increase Risk of Early-onset Cancers
Cancer is considered a disease of aging, but in recent years, there has been an alarming increase of diagnoses in people under age 55. A study presented at the Annual Meeting suggests that accelerated aging—where a person’s biological age is greater than their chronologic age—may partially explain this trend.
Ruiyi Tian, MPH, a graduate student at Washington University School of Medicine in St. Louis, reported that individuals born in or after 1965 had a 17% higher likelihood of accelerated aging than those born between 1950 and 1954, and accelerated aging, measured in this study using nine biomarkers, was associated with greater risk of early-onset lung, gastrointestinal, and uterine cancers.
“By examining the relationship between accelerated aging and the risk of early-onset cancers, we provide a fresh perspective on the shared etiology of early-onset cancers,” Tian said. “If validated, our findings suggest that interventions to slow biological aging could be a new avenue for cancer prevention, and screening efforts tailored to younger individuals with signs of accelerated aging could help detect cancers early.”
A Personalized Vaccine for Pancreatic Cancer Shows Continued Benefit
Personalized cancer vaccines can boost antitumor immunity, but their bespoke manufacturing process can be time-consuming. Using an mRNA-based vaccine platform—like the one used to develop the first COVID-19 vaccines—can shorten manufacturing time and make this treatment available to patients sooner.
Vinod Balachandran, MD, an oncologist at Memorial Sloan Kettering Cancer Center in New York City, used this approach to develop a personalized vaccine to treat pancreatic cancer. The vaccine, autogene cevumeran, is designed to target 20 proteins unique to each patient’s tumor.
At last year’s Annual Meeting, Dr. Balachandran reported that eight of 16 patients who received the vaccine in combination with other therapies developed vaccine-induced immune responses. This year, he shared that, three years after vaccination, patients who had a response to the vaccine were less likely to have experienced disease relapse, and vaccine-induced immune cells persisted and remained active in six of these patients.
“The findings that individualized neoantigen-specific cancer vaccines can induce a robust immune response that correlates with delayed disease recurrence continues to support these vaccines as an encouraging therapeutic approach for pancreatic cancer,” said Dr. Balachandran.
A Culturally Sensitive Video Raises Awareness About Prostate Cancer
Cancer screening can reduce mortality by detecting cancers early when they are more easily treated. Unfortunately, screening rates remain low for some cancers, including prostate cancer.
Mallorie Jones, MA, a project manager at the University of Pennsylvania in Philadelphia, explained that low screening rates—particularly among Black men, who have the highest rates of prostate cancer—may be partially due to limited awareness of prostate cancer risk and screening options.
To raise awareness, Jones and colleagues developed a short video capturing a conversation between a urologist and a Black pastor with the goal of providing information from trusted sources in an easily accessible format. They tested the video on 619 men, nearly half of whom were Black, from local communities.
After watching the video, the percentage of participants who knew that Black men have the greatest risk of being diagnosed with and dying of prostate cancer increased from 74% to 97%. The video also increased awareness of prostate cancer screening options and recommendations, and after watching, 93% of participants said they were interested in undergoing screening.
Innovative Methods Detect Early-stage Ovarian and Pancreatic Cancers
There are no effective screening methods for ovarian or pancreatic cancer, and because early symptoms of these cancers can be mistaken for other conditions, most patients aren’t diagnosed until their cancers have already advanced to deadlier stages.
Emerging evidence suggests that early signs of cancer can be found in the blood, meaning a simple blood test could someday screen for hard-to-find cancers—an approach known as liquid biopsy.
At the Annual Meeting, Jamie Medina, PhD, a postdoctoral fellow at the Johns Hopkins Kimmel Cancer Center in Baltimore, shared results from a study of an ovarian cancer liquid biopsy that utilizes artificial intelligence to analyze DNA fragments and protein biomarkers in the blood. Since the size and number of DNA pieces released by cancer cells into blood differ from those released by healthy cells, changes to DNA fragments can serve as a cancer biomarker. Dr. Medina reported that their approach detected 69% of stage 1 ovarian cancers.
In another presentation, Caiming Xu, PhD, a postdoctoral fellow at City of Hope Comprehensive Cancer Center in Duarte, California, shared results from a study of a liquid biopsy that looks for pancreatic cancer-specific genetic material encased in specialized vesicles called exosomes, which are released by cells into blood. Dr. Xu reported that combining analysis of exosomes with the pancreatic cancer biomarker CA19-9 accurately detected 97% of stage 1 and 2 pancreatic cancers.
KRAS Inhibition Shows Clinical Efficacy Against Colorectal Cancers
Approximately 4% of colorectal cancers harbor a genetic alteration known as a KRAS G12C mutation that makes the cancer more aggressive. Results from a phase II clinical trial reported by Scott Kopetz, MD, PhD, a professor and associate vice president at the University of Texas MD Anderson Cancer Center in Houston, suggest that blocking the activity of this mutation could be effective when combined with another targeted therapy.
In the KRYSTAL-1 trial, 94 patients with advanced KRAS G12C-mutated colorectal cancer were treated with the KRAS G12C inhibitor adagrasib (Krazati) in combination with the EGFR inhibitor cetuximab (Erbutix). The combination led to responses in 34% of patients and disease control in about 85% of patients. Patients survived for a median of 15.9 months after treatment. The results were concurrently published in the AACR journal Cancer Discovery.
“Adagrasib plus cetuximab may be a potential new standard of care for patients with previously treated KRAS G12C-mutated colorectal cancer,” Dr. Kopetz said. “Our study … underscores the importance of ongoing research to refine and expand treatment options for patients with colorectal cancer.”