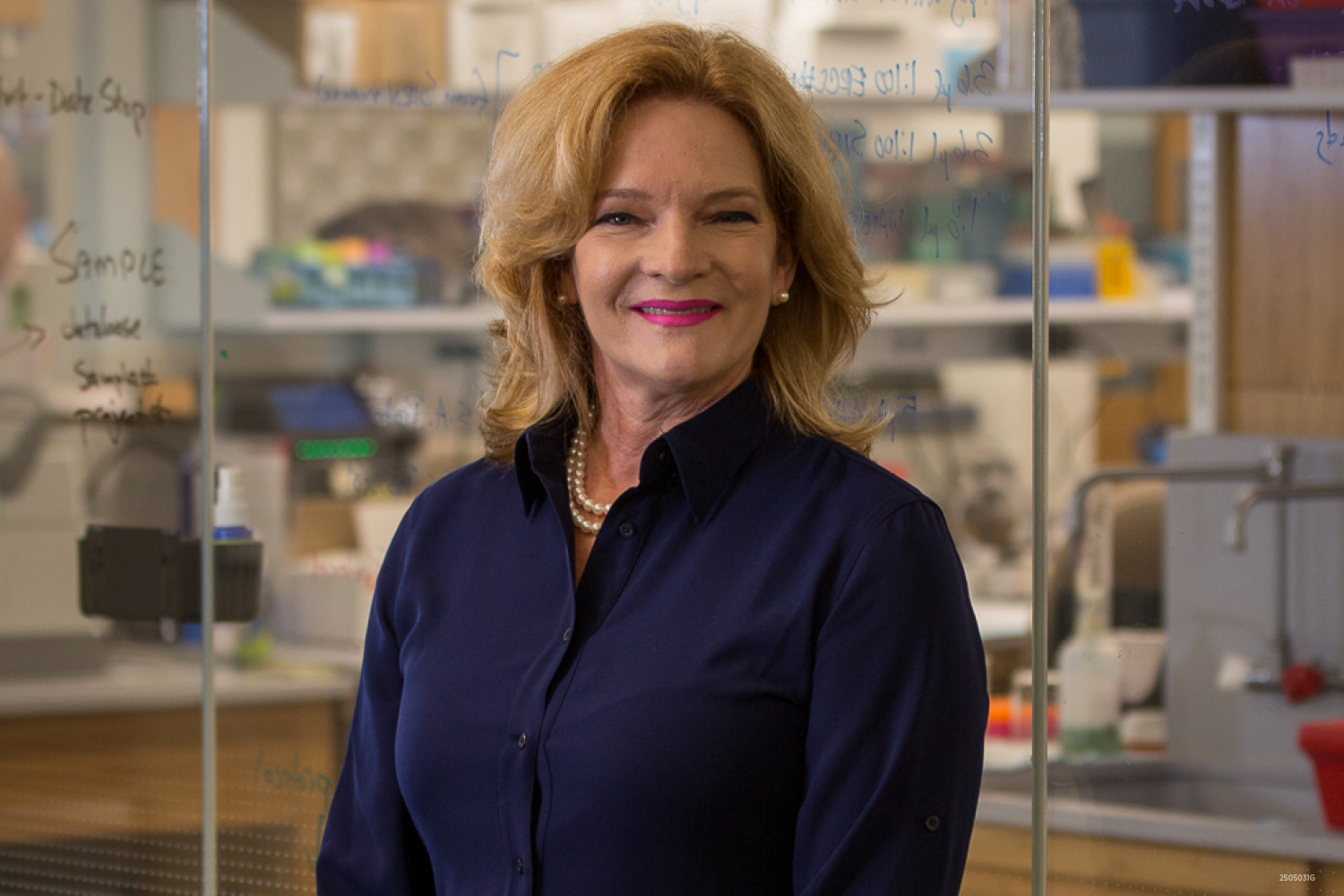
Dr. Elaine R. Mardis: Cancer Genome Pioneer
Drawn to the development of sequencing technologies, Dr. Mardis has been at the leading edge of applying next-generation sequencing to understand the genetic blueprint of cancer.
Elaine R. Mardis, PhD, recalls wanting to be a scientist at an early age. “The idea formed quite early, although I wasn’t really sure what ‘being a scientist’ meant,” she said. She was curious and drawn to science, and to chemistry in particular, thanks to her father, a chemistry teacher at the local junior college in western Nebraska where Dr. Mardis grew up.
She was also surrounded by inspiring science teachers in high school, many of whom were friends of her parents. “High school was when my interest around science came to life,” said Dr. Mardis, now the co-executive director of the Steve and Cindy Rasmussen Institute for Genomic Medicine at Nationwide Children’s Hospital in Columbus, Ohio, a Rasmussen Nationwide Foundation Endowed Chair in Genomic Medicine, and a professor of pediatrics at the Ohio State University College of Medicine.
Dr. Mardis entered the University of Oklahoma in Norman as an undergraduate majoring in zoology in 1980. She was in the honors program and worked in a laboratory doing classic genetics studies using the fruit fly, Drosophila melanogaster.
In 1984, her senior year, she took a molecular biology course that captured her imagination. “The molecular biology course really captivated me. It was tangible—the ability to purify DNA and see it on a gel,” she said.
Hooked on molecular biology just as the field of genomics was beginning to take shape, Dr. Mardis thought she would become a genetic counselor, a new discipline with only a few programs available in the U.S. She sought advice from Bruce Roe, PhD, a professor of chemistry and biochemistry, who convinced her to join his lab to pursue a PhD rather than a genetic counseling career.
Plunging Into Modern Genetics Technology
Dr. Roe, Dr. Mardis’ PhD advisor, had learned Sanger sequencing from Frederick Sanger, PhD, during a sabbatical at the Medical Research Council in England. Developed by Dr. Sanger and his colleagues in 1977, this technology was a revolutionary way to determine the sequence of DNA, for which Dr. Sanger was awarded his second Nobel Prize in Chemistry.
Dr. Roe was among the first to bring the new technique to the U.S. from England. “I often quip that I am two degrees of separation from Fred Sanger,” said Dr. Mardis.
Dr. Mardis essentially grew up in the exciting field of genomics as it emerged and expanded. In particular, she was interested in the intersection of engineering and biology. Sequencing was a labor-intensive effort, and Dr. Mardis focused on developing DNA sequencing automation using robotics to enhance its scalability. By the mid-1980s, fluorescent nucleotides were swapped for radioactivity in Sanger sequencing, and instrumentation devised in the laboratory of Leroy Hood, MD, PhD, was commercialized. According to Dr. Mardis, Dr. Roe’s academic lab was the first to acquire the new commercially available fluorescence-based DNA sequencers from Applied Biosystems. Dr. Mardis’ thesis projects included developing protocols for using the sequencer and scaling DNA sequencing efforts toward specific sequencing targets. In 1989, she published one of the first manuscripts outlining a sequencing approach for fluorescent sequencing. “I’ve always been interested in the technology of genomics and the aspects of DNA sequencing that we now take for granted—high throughput and fast turnaround. It wasn’t fast back then! My path was a little unconventional [for a] PhD, but definitely where I wanted to be.”
After completing her doctorate in 1989, Dr. Mardis wanted to continue her work in developing genomics technology. She joined Bio-Rad as a senior staff scientist in California. Bio-Rad is a life sciences research and technology company that develops and sells molecular biology assays, kits, and instruments for laboratory experiments and clinical diagnostics.
At the time, there were already discussions about the idea of a Human Genome Project—an international effort by the scientific community to map and sequence the entire human genome. Four years later, in 1993, Dr. Mardis had the opportunity to join the Genome Sequencing Center (GSC) at Washington University in St. Louis (now the McDonnell Genome Institute), to oversee Technology Development with a focus on automation and scaling the data production pipeline. The GSC had been funded by the National Human Genome Research Institute (NHGRI) as a large-scale genomic center to sequence the genome of the roundworm, C. elegans, an important model organism for studying development and neurobiology. This pilot project was meant to establish workflows for the Human Genome Project.
“Back then, there were no companies offering automation solutions for genomics. We had to design and build automated platforms to achieve the needed scale of operations for the Human Genome Project without compromising data quality. It was fun and very worthwhile,” Dr. Mardis recalled. She directed a team of engineers and molecular biology technicians on these automation and technology development projects, which contributed to the C. elegans project, done in collaboration with a team led by John Sulston, PhD, of the Wellcome Sanger Institute in Cambridge, England. The collaborators published the C. elegans genome in 1998 in Science, and then turned their attention to the much larger-scale Human Genome Project.
This international collaboration involved at least 20 institutes around the world, including in the U.S., United Kingdom, Japan, France, Germany, and China. Largely hailed as the scientific equivalent of the moonshot, this herculean project was completed in April 2003. The contributions of the Washington University GSC included organizing the BAC tiling paths needed for efficient clone-based sequencing, the production of sequencing data for approximately 20% of the genome, and the finished high-quality sequences of the Y chromosome as well as chromosomes 2, 4 and 7.
The Human Genome and Cancer
Even while working on the Human Genome Project, Dr. Mardis was being approached by “visionary people who could see the genome coming and who really wanted to use the information to understand their disease of focus. Most of those people were focused on cancer,” said Dr. Mardis.
One of those visionaries was Harold Varmus, PhD, then the president of Memorial Sloan Kettering Cancer Center in New York City. Dr. Varmus and one of his trainees, William Pao, MD, PhD, wanted to understand why some lung cancer patients responded well to new small molecule-based therapies, while others had no response. Dr. Mardis and her colleagues collaborated with Drs. Varmus and Pao by sequencing selected genes from lung cancer patient samples with known response or resistance. In 2004, they reported a distinct set of EGFR mutations in patients that were sensitive to the targeted therapies. Shortly thereafter, they identified a key resistance mutation to these therapies. The findings sparked Dr. Mardis to focus on using sequencing technology and the human genome reference to probe the biology of cancer.
Timothy J. Ley, MD, a hematologist and cancer biologist also at Washington University, was another visionary who had been “bothering us all while we were finishing the human genome,” Dr. Mardis recalled jokingly. Dr. Ley treated patients with acute myeloid leukemia (AML) and wanted to understand the genetic basis for why his patients were developing leukemia. It was the mid-2000s, and next generation sequencing had just emerged, allowing researchers to generate DNA sequences significantly faster than with Sanger sequencing. Dr. Mardis’ group was among the first to have these new sequencers. “The benefit of developing technology at a genome center at the forefront of genomics was that we were the first door that companies knocked on, because we were the opinion leaders in the field. They really wanted to get their instrument in the door and have us try it,” said Dr. Mardis.
The GSC had already begun using PCR and Sanger sequencing to study potentially mutated genes using DNA from cancerous bone marrow cells from AML patients to identify frequently mutated genes.
Dr. Mardis recalled thinking how slowly this approach was taking to pace through sequencing the genes that Dr. Ley had identified as potential drivers of AML in a large patient cohort. Considering the next generation technology, they decided to try sequencing the entire AML and matched normal genome from one patient. Ultimately, they received private funding for the effort, which was published in a landmark paper in Nature in 2008. It was a watershed moment in cancer research—the first sequenced genome of a cancer patient and the first side-by-side comparison of a cancer genome and a normal tissue genome from the same person.
“The publication showed that we could sequence a cancer genome, compare the sequences to those from a matched normal tissue, and identify mutations unique to the cancer as a means to understand the cancer drivers without having to guess which genes we should study,” explained Dr. Mardis.
A year later, in 2009, the team at Washington University followed up with a second publication that identified mutations in IDH1 (encoding isocitrate dehydrogenase 1) in a second AML patient that were shown to be recurrent across a panel of 180 AML samples. This study emerged only a few months after these IDH1 mutations were identified in gliomas, a type of brain cancer, by the laboratory of Bert Vogelstein, MD, of Johns Hopkins University. These discoveries, in turn, led to effective targeted therapies for both cancer types.
A Singular Cancer Genome Researcher
Dr. Mardis had also established a collaboration with breast cancer oncologist and researcher Matthew Ellis, MD, PhD, now the senior vice president of clinical development precision oncology at Guardant Health, who was then at Washington University. Dr. Ellis wanted to characterize mutations causing various types of breast cancer and had been collecting patient samples from clinical trials. In 2010, Drs. Ellis and Mardis reached a new cancer research milestone: They published a paper in Nature comparing not only the whole genome of a primary tumor—a basal-like breast cancer (a type of triple-negative breast cancer)—to corresponding normal tissue, but also a brain metastasis and xenografted primary tumor from the same patient.
“For the first time, we demonstrated that xenografted tumors recapitulated the human disease. This cancer was also the first to be sequenced from an African American patient,” Dr. Mardis said.
In 2012, Drs. Mardis and Ellis followed up the work with yet another Nature paper, this time on the whole genomes of estrogen receptor (ER)-positive breast cancers collected on a clinical trial of aromatase inhibitor therapy. Their findings helped inform which genomic features in ER-positive disease predicted benefit from neoadjuvant treatment with aromatase inhibitors.
In parallel with many ongoing cancer genomics projects, Dr. Mardis and her computational colleagues at Washington University were devising cancer genomics-based analytical approaches that included tools to characterize clonality changes across treatment intervals or between primary and metastatic disease samples, to identify structural variants, and to identify neoantigens that could be used in personalized vaccine approaches.
The McDonnell Genome Institute, as one of the large-scale NHGRI centers, played a key role in The Cancer Genome Atlas (TCGA) program, a multidisciplinary effort of the National Cancer Institute and the NHGRI, which created a multi-omics data set of primary cancer and matched normal samples across 33 cancer types. Dr. Mardis co-led the analysis of the TCGA endometrial cancer genome project. One result of this study demonstrated that patients with mutations in the gene for an enzyme involved in DNA replication called polymerase epsilon had higher overall mutation rates in their tumor genomes, but also better outcomes, compared to other patients with endometrial cancers.
Dr. Mardis also co-led the Pediatric Cancer Genome Project, a collaboration between St. Jude Children’s Research Hospital and the McDonnell Genome Institute. This project profiled over 800 pediatric cancers in a five-year program, revealing novel drivers and other characteristics unique to pediatric cancers.
The publication showed that we could sequence a cancer genome, compare the sequences to those from a matched normal tissue, and identify mutations unique to the cancer as a means to understand the cancer drivers without having to guess which genes we should study.”
–Elaine R. Mardis, PhD
In 2016, Dr. Mardis was recruited with Richard Wilson, PhD, to Nationwide Children’s Hospital (NCH), where they founded the Institute for Genomic Medicine (IGM). Dr. Mardis serves as co-executive director of IGM and is also a professor of pediatrics at the Ohio State University College of Medicine. “The move to Nationwide Children’s was to fully integrate genomics into the diagnosis and medical care of pediatric patients, across multiple specialty clinics including cancer.”
Dr. Mardis has brought her eye for efficiency, detail, and team science-based collaboration to Nationwide Children’s. Unlike adult cancers, pediatric cancers have fewer mutations in the genome. Instead, pediatric cancers are more likely to have copy number changes that are important for risk prognostication and to harbor gene fusion drivers as well as epigenetic signatures, all of which impact diagnostic accuracy. To this end, she and her IGM colleagues developed a research study aimed at developing and applying complex DNA- and RNA-based profiling along with methylation array-based classification to NCH cancer patients.
After studying an initial cohort of more than 290 pediatric cancer patients between 2018 and 2022, these assays were clinically validated in the IGM Clinical Laboratory that serves the NCH patient population. This expertise and capacity qualified the IGM team to compete for and be awarded an NCI contract for a much more ambitious project that launched in March 2022, in collaboration with the Children’s Oncology Group (COG), called the Molecular Characterization Initiative (MCI). There are 226 COG affiliates in the U.S., Canada, Australia, and New Zealand, most of which have enrolled patients onto MCI.
Every patient who participates in MCI enrolls into a COG-led registry called Project Every Child. The patient’s tumor and blood samples are collected, tested and analyzed at NCH. The clinical results are then used to make treatment and clinical care decisions, including clinical trial enrollment. “We are so proud of our MCI work in making comprehensive profiling broadly available, especially for those who would not normally be able to access these tests,” Dr. Mardis noted. The time from receipt of samples to clinical results is just 21 days—remarkably fast given the complexity of the process and, importantly, within the time frame when clinical care decisions typically occur.
The pooled MCI data and results are de-identified and submitted to the NCI’s Childhood Cancer Database, enabling future discoveries through publicly available access. Three years into the project, the MCI has more than 5,500 participants (ages 0-25) and is creating ever clearer characterization of pediatric and AYA cancers, including many rare cancers that have been difficult to study beyond case studies because there are so few children with these cancers. As the number of tumor subcategories grow, clinicians and researchers have new information to better treat and develop novel treatments for children with cancer. Regarding MCI, Dr. Mardis said, “Our work has tangible benefits for patients’ lives every day and that is just super rewarding.”
For Dr. Mardis, one rewarding aspect of the work is providing clinically useful information to pediatric oncologists in real time so that they can make clinical decisions. “It’s also exciting to generate and deposit the data into the Childhood Cancer Database because the collective data are potentiating innovative research on pediatric cancers and hopefully identifying new therapeutics. We’re very excited about that.”
For example, Nationwide Children’s pediatrics researcher Genevieve Kendall, PhD, is introducing MCI-identified gene fusions among soft tissue sarcoma samples into zebrafish to produce new models of sarcoma, with an aim to understand how these fusions drive sarcoma biology. “Dr. Kendall’s efforts are exemplary of the research for which the MCI data should be used,” said Dr. Mardis.
AACR Contributions
 Elaine R. Mardis, PhD, has been an active member of the American Association for Cancer Research® (AACR) since 2009. In 2019, just a decade later, she was inaugurated as AACR president. The same year, Dr. Mardis was elected to the Fellows of the AACR Academy and was named a member of the National Academy of Medicine. Her time as AACR president was notable because the COVID-19 pandemic hit the U.S. in March 2020 toward the end of her one-year term, forcing the AACR to quickly pivot the AACR Annual Meeting in April from an in-person event to a virtual one. In 2021, Dr. Mardis was named a founding editor-in-chief, along with Lillian L. Siu, MD, of a new AACR journal titled Cancer Research Communications.
Elaine R. Mardis, PhD, has been an active member of the American Association for Cancer Research® (AACR) since 2009. In 2019, just a decade later, she was inaugurated as AACR president. The same year, Dr. Mardis was elected to the Fellows of the AACR Academy and was named a member of the National Academy of Medicine. Her time as AACR president was notable because the COVID-19 pandemic hit the U.S. in March 2020 toward the end of her one-year term, forcing the AACR to quickly pivot the AACR Annual Meeting in April from an in-person event to a virtual one. In 2021, Dr. Mardis was named a founding editor-in-chief, along with Lillian L. Siu, MD, of a new AACR journal titled Cancer Research Communications.
Dr. Mardis cares deeply about education and continues to develop translational research curricula for the AACR for cancer biologists and researchers at every stage of their careers. Dr. Mardis is one of three directors of an upcoming AACR translational cancer workshop for basic scientists. Her mentoring philosophy is to “find really bright individuals who know what they want to do and give them the freedom to do it. If they need me to roll up my sleeves and help along the way and discuss strategies, that is fine. Younger people now are so smart that I’m not going to stand in their way! I’m here to guide and offer advice and provide the resources. That is a formula that works for me and for the people whom I’m training. So far, so good.”
 Cover Art:
Cover Art:
Dr. Elaine R. Mardis’ seminal work on the Human Genome Project led her to contribute to other large-scale genomics projects, including The Cancer Genome Atlas and the Pediatric Cancer Genome Project. Today, she is leading a nationwide effort to generate and analyze clinical molecular profiles of pediatric and adolescent/young adult patients in collaboration with the National Cancer Institute and Children’s Oncology Group. The de-identified data from this project are publicly available in the Childhood Cancer Database, fueling future discoveries in pediatric cancer biology and treatment.
Illustration ©2025 AACR/SayoStudio