Research Updates
The Search for Pancreatic Cancer’s Weaknesses
 The American Association for Cancer Research® (AACR) held its annual Special Conference on Advances in Pancreatic Cancer September 15 to 18, 2024, in Boston. In their keynote lectures, Eileen O’Reilly, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York City, and Joseph Mancias, MD, a radiation oncologist at Dana-Farber Cancer Institute in Boston, shared how studying pancreatic cancer’s strengths can help reveal its weaknesses.
The American Association for Cancer Research® (AACR) held its annual Special Conference on Advances in Pancreatic Cancer September 15 to 18, 2024, in Boston. In their keynote lectures, Eileen O’Reilly, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York City, and Joseph Mancias, MD, a radiation oncologist at Dana-Farber Cancer Institute in Boston, shared how studying pancreatic cancer’s strengths can help reveal its weaknesses.
Dr. O’Reilly described recent advances in targeted therapy for pancreatic cancer. These included clinical trials in which patients whose tumors have mutations in BRCA1/2, KRAS, or other genes have been successfully matched with drugs designed to target such tumors.
Dr. Mancias explained how pancreatic tumors use a recycling process called autophagy to free up iron that tumors need to grow. He and his colleagues have found that pancreatic cancer cells boost production of the protein NCOA4, which draws the iron-storage protein ferritin into the cell’s autophagy machinery. This degrades ferritin, releasing free iron. Researchers are developing various ways to block this process, some of which are currently being tested in clinical trials.
Pinpointing the Causes of Childhood Cancer
 If cancer is typically the product of decades of accumulated cellular damage, how does cancer arise in children? Experts at the AACR Special Conference on Advances in Pediatric Cancer Research, held September 5 to 8, 2024, in Toronto, discussed the genetic drivers of childhood cancer and how researchers are working to target them.
If cancer is typically the product of decades of accumulated cellular damage, how does cancer arise in children? Experts at the AACR Special Conference on Advances in Pediatric Cancer Research, held September 5 to 8, 2024, in Toronto, discussed the genetic drivers of childhood cancer and how researchers are working to target them.
Presentations included new ways to tailor treatments for children with syndromes that predispose them to get cancer, such as Li-Fraumeni syndrome. Among the strategies are monitoring the risks of secondary cancers after radiation in patients with Li-Fraumeni syndrome and combining different immune checkpoint inhibitors in patients with constitutional mismatch repair deficiency syndrome.
Researchers also discussed the benefits of genetic screening for children with cancer to identify cancer predisposition syndromes and evaluate eligibility for targeted therapies. In one study, universal access to whole-genome sequencing for cancers diagnosed in patients before age 25 gave 29% of these patients additional clinically relevant information beyond traditional diagnostics. But with an increase in genomic testing and information, experts cautioned, comes the responsibility to balance the potential benefits with the financial costs and emotional uncertainty for patients and their families.
Pediatric Lymphoma Versus Adult Lymphoma
 Lymphomas are most commonly diagnosed in children and young adults or in patients 60 and older. At the Advances in Malignant Lymphoma: Maximizing the Basic-Translational Interface for Clinical Application conference, organized by the AACR in partnership with the International Conference on Malignant Lymphoma and held June 19 to 22, 2024, in Philadelphia, researcher Lisa G. Roth, MD, discussed how Hodgkin lymphoma cases differ between young and old patients.
Lymphomas are most commonly diagnosed in children and young adults or in patients 60 and older. At the Advances in Malignant Lymphoma: Maximizing the Basic-Translational Interface for Clinical Application conference, organized by the AACR in partnership with the International Conference on Malignant Lymphoma and held June 19 to 22, 2024, in Philadelphia, researcher Lisa G. Roth, MD, discussed how Hodgkin lymphoma cases differ between young and old patients.
Dr. Roth, the director of pediatric oncology at Weill Cornell Medicine in New York City, and her colleagues sequenced the full genomes of lymphoma cells from patients from two age groups: 7 to 17 and 55 to 85. Cells in younger patients had significantly more mutations than cells from older patients, chiefly driven by two “clock-like” mutation signatures that promote the accumulation of mutations over time.
Dr. Roth emphasized that more knowledge about these different mutational patterns may help researchers better estimate prognosis and guide treatment strategies. She suggested grouping patients based on the biology of their disease rather than as “pediatric” and “adult.”
AACR Conference on The Science of Cancer Health Disparities
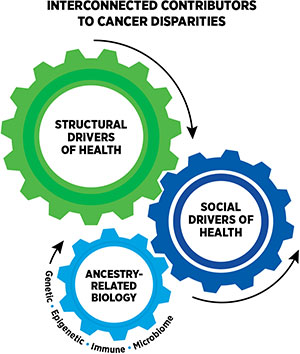
From September 21 to 24, 2024, researchers gathered in Los Angeles for the 17th AACR Conference on The Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved to discuss inequities in cancer care and how to help close the gaps. Presented studies ranged from genome-wide comparisons between groups to large-scale analyses of the cultural and socioeconomic systems that affect health care.
For instance, researchers in one study assessed how symptoms related to sexual health among Black and white patients receiving hormone therapy for breast cancer were related to treatment adherence. Janeane N. Anderson, PhD, MPH, a researcher at the University of Tennessee Health Science Center in Memphis, and colleagues found that sexual health symptoms were associated with poorer mental quality of life in both Black and white patients, but they were associated with poorer physical quality of life and poorer treatment adherence in Black patients only.
Racial disparities may also exist when it comes to treatment, according to a study presented by Jincong Q. Freeman, MPH, a PhD candidate at the University of Chicago. Using a database of clinical and demographic features from more than 10,000 patients with triple-negative breast cancer, Freeman and colleagues found that Black patients with early-stage and metastatic disease were 11% and 37% less likely to receive immunotherapy than
white patients with similar-stage disease.
But there is hope for policies that may help close treatment gaps, argued Sriya Kudaravalli, a medical student at the University of Pittsburgh School of Medicine. Kudaravalli and colleagues investigated whether the passage of the Affordable Care Act (ACA) impacted which patients with stage 3 colon cancer receive care concordant with practice guidelines. After ACA implementation, from 2014 to 2019, the receipt of guideline-concordant care increased by an average of 7.8% per year for non-white patients, 7.7% per year for those in rural areas, and 3.5% per year for patients in the most socioeconomically disadvantaged neighborhoods.
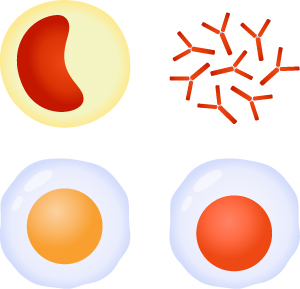
Risk of New Cancers After CAR T Comparable to Risk After Other Therapies
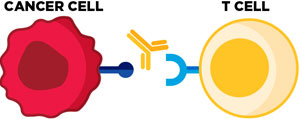
In November 2023, the Food and Drug Administration (FDA) announced it was launching an investigation into the risk of developing new T-cell cancers after treatment with chimeric antigen receptor T-cell (CAR T) therapy, a type of immunotherapy.
Kai Rejeski, MD, a research fellow at Memorial Sloan Kettering Cancer Center in New York City, and colleagues performed a meta-analysis, which they published in the AACR journal Clinical Cancer Research. In a total of 5,517 adult patients with lymphoma or multiple myeloma who received one of the six FDA-approved CAR T therapies, 5.8% developed a second cancer, with only 0.09% developing a T-cell cancer. In a subset of 1,253 patients from studies that compared CAR T to other cancer treatments, 5% of patients treated with CAR T developed a second cancer, compared to 4.9% of patients treated with other standard therapies.
“These data do not suggest that there is an increased risk of [secondary cancers] relative to other standard-of-care therapies,” Dr. Rejeski said.
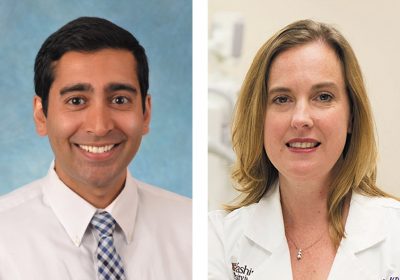
Immunotherapy May Facilitate Surgery for Patients With High-risk Liver Cancer
 Only around 30% of patients with early-stage liver cancer are eligible for surgery because of factors such as tumor size, proximity to important structures, and safety concerns, explained Mark Yarchoan, MD, an oncologist at the Johns Hopkins Kimmel Cancer Center in Baltimore.
Only around 30% of patients with early-stage liver cancer are eligible for surgery because of factors such as tumor size, proximity to important structures, and safety concerns, explained Mark Yarchoan, MD, an oncologist at the Johns Hopkins Kimmel Cancer Center in Baltimore.
In a study published in the AACR journal Cancer Research Communications, Dr. Yarchoan and colleagues investigated whether immunotherapy given before surgery, also called neoadjuvant immunotherapy, may mitigate some of the high-risk features and make surgery safer and more effective in these patients. They looked at outcomes from 92 patients who had their liver cancer surgically removed. This included 36 patients who received neoadjuvant immunotherapy, 61.1% of whom would not have been candidates for surgery based on traditional eligibility criteria.
Nearly 95% of patients who received neoadjuvant immunotherapy underwent successful surgery with cancer-free margins. Further, patients who received neoadjuvant immunotherapy before surgery lived a median of 44.8 months without a cancer recurrence, compared to 49.3 months among patients treated with up-front surgery. “There is a group of patients with high-risk liver cancer who, in a contemporary era, may have long-term survival through aggressive treatment with systemic therapy followed by surgery,” Dr. Yarchoan said.
HPV Testing at Longer Intervals May Still Effectively Detect Cervical Cancer
 The U.S. Preventive Services Task Force (USPSTF) currently recommends that people with a cervix receive either cytology screening (such as a Pap test) every three years, screening for HPV every five years, or both every five years. However, some experts have raised concerns that the extended interval between HPV tests may miss some precancerous lesions before they turn into cervical cancer, according to Anna Gottschlich, PhD, MPH, an epidemiologist at the Karmanos Cancer Institute in Detroit.
The U.S. Preventive Services Task Force (USPSTF) currently recommends that people with a cervix receive either cytology screening (such as a Pap test) every three years, screening for HPV every five years, or both every five years. However, some experts have raised concerns that the extended interval between HPV tests may miss some precancerous lesions before they turn into cervical cancer, according to Anna Gottschlich, PhD, MPH, an epidemiologist at the Karmanos Cancer Institute in Detroit.
Dr. Gottschlich and colleagues found that the risk of developing precancerous lesions within three years after a negative HPV test was similar to the risk within eight years after a negative HPV test—0.33% and 0.32%, respectively. These data suggest that lengthening the interval between recommended HPV tests may be safe for some patient populations. Gottschlich said this not only supported the robustness of HPV testing but may help better inform screening guidelines as HPV testing gains traction in the United States.