Research Updates
AACR Launches Kidney Cancer Conference
 The American Association for Cancer Research® (AACR) held its first-ever Special Conference on Advances in Kidney Cancer Research June 24 to 27, 2023, in Austin, Texas. Laboratory and clinical researchers convened to discuss important topics such as identifying new drug targets in kidney cancer, targeting cell metabolism and regulating gene expression, and using immunotherapies, alone or in combination, to treat kidney cancer.
The American Association for Cancer Research® (AACR) held its first-ever Special Conference on Advances in Kidney Cancer Research June 24 to 27, 2023, in Austin, Texas. Laboratory and clinical researchers convened to discuss important topics such as identifying new drug targets in kidney cancer, targeting cell metabolism and regulating gene expression, and using immunotherapies, alone or in combination, to treat kidney cancer.
In an interview with Cancer Research Catalyst, the official AACR blog, conference co-chair M. Celeste Simon, PhD, scientific director of the Abramson Family Cancer Research Institute at the University of Pennsylvania in Philadelphia, stated that the conference was designed for all kidney cancer researchers. “Special conferences provide an ideal platform for scientists to really connect and talk with everyone,” she said. “This meeting was conceived with the goal of bringing together investigators from the entire spectrum of research on kidney cancer.”
Cutting-edge Advances in Head and Neck Cancer Research
 In July 2023, the AACR and the American Head and Neck Society (AHNS) co-hosted the third AACR-AHNS Head and Neck Cancer Conference: Innovating Through Basic, Clinical, And Translational Research, which took place in Montreal. Head and neck cancers affect the throat, nose, nasal sinuses, salivary glands, and nerves and muscles in the head and neck.
In July 2023, the AACR and the American Head and Neck Society (AHNS) co-hosted the third AACR-AHNS Head and Neck Cancer Conference: Innovating Through Basic, Clinical, And Translational Research, which took place in Montreal. Head and neck cancers affect the throat, nose, nasal sinuses, salivary glands, and nerves and muscles in the head and neck.
Select presentations offered innovative ideas for detecting these tumors earlier. One study showed that detection of DNA from the human papillomavirus (HPV), a common cause of head and neck squamous cell carcinoma (HNSCC), in an individual’s bloodstream could help predict HNSCC five to 10 years before current methods detect a tumor. Another study demonstrated how to better predict HNSCC recurrences after surgery by scanning for tumor DNA in the surgical drain, which could reveal if tumor cells remain at the surgical site or in nearby lymph nodes.
Other studies presented ideas for making treatments more effective. In one presentation, researchers showed that immunotherapy given before surgery allows the immune system to mount a more sustained response against a tumor than when given after surgery. Another researcher showed that an investigational drug designed to boost the dose of radiation that cancer cells receive can also enhance the immune stimulatory effects of radiation, helping the immune system to fight cancer.
Electrical Signaling Between Skin Cells May Affect Melanoma Development
 In zebrafish, mouse, and human cell models, researchers discovered that the transfer of neurotransmitters from one type of skin cell to another promoted the development of melanoma. The study was published in the AACR journal Cancer Discovery on October 5, 2023.
In zebrafish, mouse, and human cell models, researchers discovered that the transfer of neurotransmitters from one type of skin cell to another promoted the development of melanoma. The study was published in the AACR journal Cancer Discovery on October 5, 2023.
Melanomas develop from skin cells called melanocytes, explained the study’s first author, Mohita Tagore, PhD, a postdoctoral research scientist at Memorial Sloan Kettering Cancer Center (MSKCC) in New York City. She and her colleagues found that melanocytes with a cancer-promoting mutation in the BRAF gene can secrete the neurotransmitter GABA when in contact with another type of skin cell called keratinocytes. This discovery surprised Richard White, MD, PhD, senior author of the study and a physician-scientist at MSKCC and the Oxford Branch of the Ludwig Institute for Cancer Research in Oxford, England, because GABA signaling is typically associated with neurons.
Drs. White and Tagore and colleagues found that the GABA secreted by mutated melanocytes silenced electrical signaling in the keratinocytes, which in turn secreted a tumor-promoting protein that could be taken up by melanocytes. The study suggested that GABA may be a potential therapeutic target in melanoma, though additional research is needed.
Benzodiazepines Associated With Varying Outcomes in Pancreatic Cancer
 In a study published in the AACR journal Clinical Cancer Research September 15, 2023, pancreatic cancer patients who took the benzodiazepine lorazepam (Ativan) did not live as long without disease progression as patients who did not take lorazepam. Conversely, pancreatic cancer patients who took the benzodiazepine alprazolam (Xanax) lived longer without disease progression.
In a study published in the AACR journal Clinical Cancer Research September 15, 2023, pancreatic cancer patients who took the benzodiazepine lorazepam (Ativan) did not live as long without disease progression as patients who did not take lorazepam. Conversely, pancreatic cancer patients who took the benzodiazepine alprazolam (Xanax) lived longer without disease progression.
Benzodiazepines are commonly prescribed during cancer treatment to ease side effects such as anxiety and insomnia. In this study, patients who took lorazepam had a 3.83-fold higher risk of disease progression or death than patients who did not, while patients who took alprazolam had a 62% lower risk of disease progression or death than patients who did not. Lorazepam was also associated with significantly worse overall survival in prostate, ovarian, head and neck, uterine, colon, and breast cancers, as well as melanoma, explained study author Michael Feigin, PhD, an associate professor of pharmacology and therapeutics at Roswell Park Comprehensive Cancer Center in Buffalo, New York.
While Dr. Feigin stressed that these data are too preliminary to change clinical practice, they suggest that lorazepam and alprazolam affect pancreatic tumors, and perhaps tumors of other origins, in different ways.
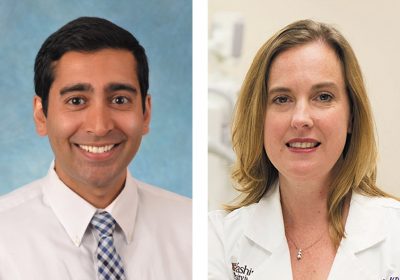
Undertaking Cost-related Administrative Tasks May Disrupt Cancer Care
 Patients with cancer who engaged in cost-related administrative tasks—such as estimating the costs of procedures or medications, appealing a denial of insurance benefits, or asking insurance companies for help—were 18% more likely to experience delayed or missed appointments, procedures, or medications. These results were published in the AACR journal Cancer Epidemiology, Biomarkers & Prevention August 30, 2023.
Patients with cancer who engaged in cost-related administrative tasks—such as estimating the costs of procedures or medications, appealing a denial of insurance benefits, or asking insurance companies for help—were 18% more likely to experience delayed or missed appointments, procedures, or medications. These results were published in the AACR journal Cancer Epidemiology, Biomarkers & Prevention August 30, 2023.
In the U.S. health care system, the burden of knowing how to use and pay for services falls to the consumer, explained study author Meredith Doherty, PhD, LCSW, an assistant professor at the University of Pennsylvania School of Social Policy & Practice in Philadelphia. She and her colleagues analyzed data from a survey that asked cancer patients and survivors about their engagement in administrative tasks, as well as their experience with care delays or nonadherence, such as postponing or skipping appointments, lab tests, or prescription refills. Those who engaged in administrative tasks were not only more likely to experience delays or nonadherence than those who did not, but each additional task increased the likelihood of delays or nonadherence by 32%. Dr. Doherty added that African Americans were more likely than other racial and ethnic groups to engage in administrative tasks and experience delays or nonadherence.
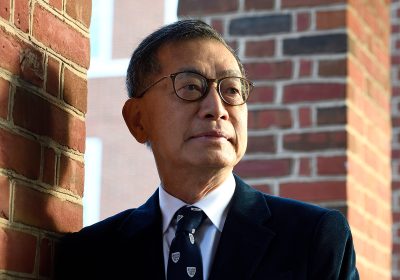
Pancreatic Cancer Conference Features Insights From Experienced and Emerging Researchers
 The keynote session of the AACR Special Conference on Pancreatic Cancer, held September 27 to 30, 2023 in Boston, featured cutting-edge research from established, up-and-coming, and early-career researchers.
The keynote session of the AACR Special Conference on Pancreatic Cancer, held September 27 to 30, 2023 in Boston, featured cutting-edge research from established, up-and-coming, and early-career researchers.
Christine A. Iacobuzio-Donahue, MD, PhD, a pathologist and director of the Center for Pancreatic Cancer Research at Memorial Sloan Kettering Cancer Center in New York City, presented her findings about how pancreas cells acquire the mutations that make them cancerous. She and her colleagues found that most mutations that drive tumor growth occur in the precancer stages before the tumor invades nearby tissue. This indicates that almost all cells in the tumor have these crucial mutations, meaning patients may benefit from targeted therapies aimed at those driver mutations, Dr. Iacobuzio-Donahue explained.
Tumors can also evolve independently of mutations, said Luisa Escobar-Hoyos, MSc, PhD, an assistant professor of therapeutic radiology at Yale School of Medicine in New Haven, Connecticut, in her Rising Star Keynote presentation. She explained that large-scale changes in RNA, including the expression of genes typically found only in embryos, may drive particularly aggressive pancreatic cancers. Some of these altered patterns of RNA expression may depend on defects in RNA processing, Dr. Escobar-Hoyos said. She and her colleagues are investigating how to target these defective processes.
The keynote session also featured two-minute Lightning Talks from graduate students and postdoctoral researchers. “This is a meeting for everyone who works in pancreas cancer,” said co-chair Anirban Maitra, MBBS, scientific director of the Sheikh Ahmed Pancreatic Cancer Research Center at the University of Texas MD Anderson Cancer Center in Houston.
Finding and Blocking New Drug Targets
 Targeted therapies, which interfere with the defective proteins that drive cancer, have made up the majority of new oncology drugs in the past 25 years. At the AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, held October 11 to 15, 2023 in Boston, researchers convened to discuss how to continue this progress.
Targeted therapies, which interfere with the defective proteins that drive cancer, have made up the majority of new oncology drugs in the past 25 years. At the AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, held October 11 to 15, 2023 in Boston, researchers convened to discuss how to continue this progress.
In a phase I trial, researchers tested a new targeted therapy against tumors deficient in the protein methylthioadenosine phosphorylase (MTAP). MTAP deficiency decreases activity of another protein, PRMT5, making cells vulnerable to additional PRMT5 inhibition by the drug AMG 193. In this phase I clinical trial of 31 patients with MTAP-deficient tumors, five patients experienced a partial response, and 14 patients experienced stable disease, explained presenter Jordi Rodon, MD, PhD, associate professor in the Department of Investigational Cancer Therapeutics at the University of Texas MD Anderson Cancer Center in Houston.
In another phase I clinical trial, researchers tested a new drug targeting KRAS, one of the most commonly mutated genes in human cancers. While currently approved drugs target a single mutation known as G12C, Alexander Spira, MD, PhD, the CEO and clinical director of NEXT Oncology Virginia, a co-director of the Virginia Cancer Specialists Research Institute, and a clinical assistant professor at Johns Hopkins University in Baltimore, and colleagues designed a drug that targets several common KRAS mutations. The drug, RMC-6236, has been given to 131 patients so far, resulting in partial responses and a decrease in the amount of mutant KRAS observed in the blood of patients with several different tumor types.
Related Posts