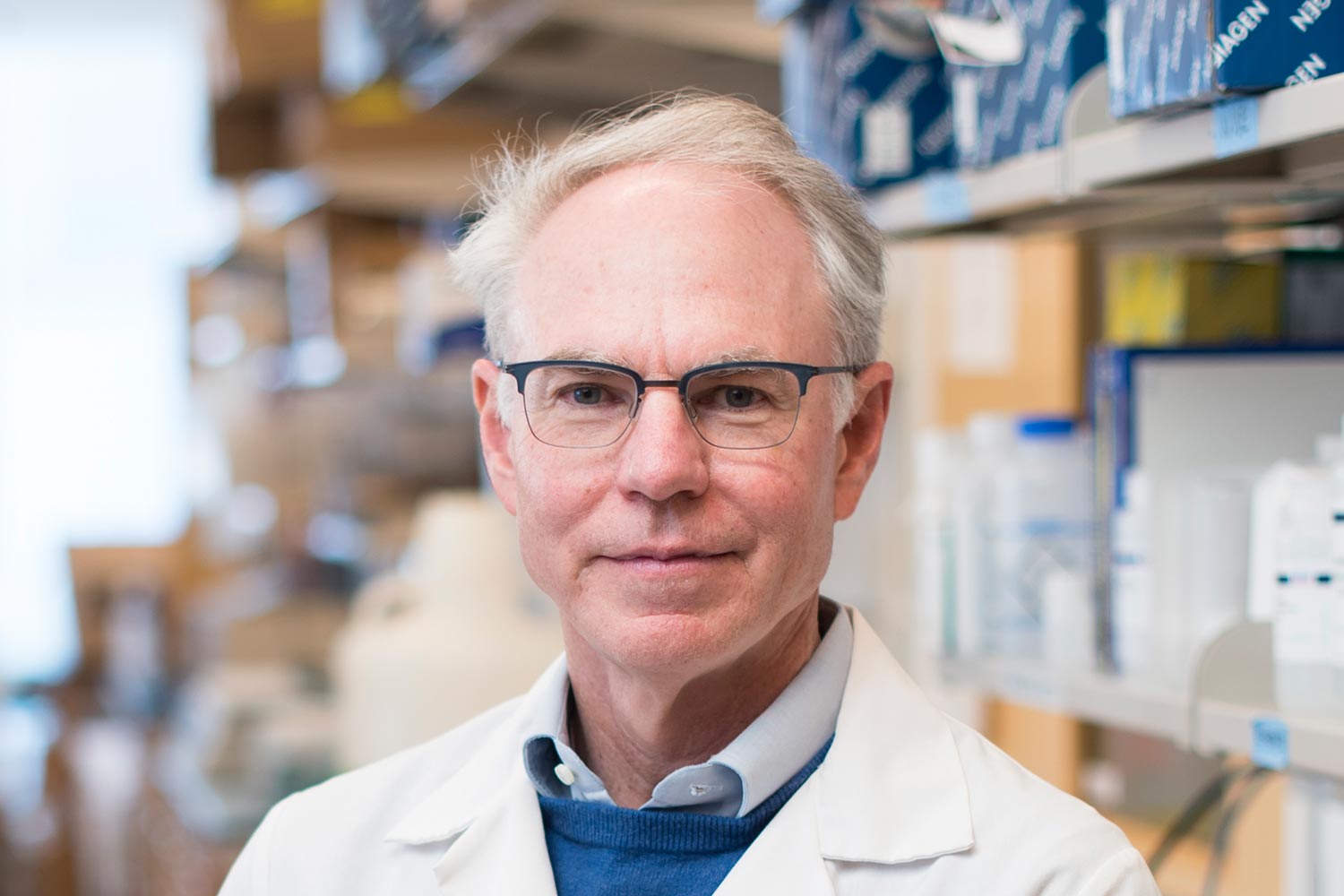
Dr. Charles L. Sawyers: At the Leading Edge of Targeted Therapies
He co-developed Gleevec, among the first targeted cancer therapies, and is set on understanding prostate cancer drug resistance.
While in medical school at Johns Hopkins University in Baltimore in the 1980s, Charles L. Sawyers’ eyes were opened to the knowledge that could be uncovered by probing the molecular biology of a disease. One of his medical school professors, a hematologist, had helped uncover the structure of the protein encoded by a hemoglobin gene that, when mutated, causes sickle cell anemia. The professor taught Sawyers and his classmates how the knowledge of the mutated protein’s structure could explain the manifestations of sickle cell anemia. That experience cemented in Sawyers a desire to understand the molecular basis of human disease.

Today, Charles L. Sawyers, MD, is a physician-scientist and chair of the Human Oncology and Pathogenesis Program at Memorial Sloan Kettering Cancer Center in New York City. But first, after he completed medical school in 1985, he headed west to begin a residency in internal medicine at the University of California, San Francisco (UCSF). While there, he experienced firsthand how molecular biology tools, including molecular cloning, were being used to figure out the biological mechanisms of certain diseases—and how to treat them. Inspired by the chronic myeloid leukemia (CML) patients he cared for at UCSF—who at the time had about three years of life left following their diagnosis—Dr. Sawyers redoubled his efforts to understand the molecular basis of their disease.
In 1988, Dr. Sawyers moved to the University of California, Los Angeles (UCLA) for a clinical fellowship. His oncology training started when the cancer field was beginning to use molecular biology to understand the causes and drivers of cancer and to apply what was learned to develop therapies that went beyond chemotherapies. In 1982, Robert A.Weinberg, PhD, at the Massachusetts Institute of Technology, had made the first discovery of a human oncogene, RAS, and Dr. Sawyers’ adviser at UCLA, Owen N. Witte, MD, had helped identify the fusion BCR-ABL gene, an oncogene that results in the development of CML. An oncogene is a gene that, when mutated, has the potential to cause cancer. In Dr. Witte’s lab in 1990, Dr. Sawyers showed that the RNA of the BCR-ABL fusion gene could be detected in the blood of CML patients, and he developed a PCR-based test to detect the molecular marker. The marker’s presence indicated relapse for CML that showed up before pathologists could detect it using traditional pathology methods. He also provided solid evidence for understanding the mechanism by which the BCR-ABL oncogene turns a normal cell into a malignant one.

In 1993, Dr. Sawyers started his own lab at UCLA and accepted an assistant professorship position at UCLA’s cancer center. He continued his research on BCR-ABL and CML, and also spent some of his time caring for patients as a hematologist-oncologist. Meanwhile, researchers, including Brian Druker, MD, a physician-scientist at the Oregon Health & Science University in Portland, had begun the hunt for a molecule that could target BCR-ABL. Dr. Druker, working with researchers at the Swiss pharmaceutical company Ciba-Geigy, already had a molecule, imatinib, that could kill leukemia cells that expressed BCR-ABL but not kill nonmalignant cells or other cancer cells that did not rely on the BCR-ABL oncogene. The imatinib data that Dr. Druker and colleagues had generated, and that he showed to Dr. Sawyers in 1995, was enough to convince Dr. Sawyers to join in on the clinical development of imatinib. Drs. Sawyers and Druker organized a clinical trial of imatinib in patients with CML who had failed to respond to standard therapy. The trial began in 1998, and imatinib was approved as Gleevec in May 2001 based on results from a phase II clinical trial, marking the fastest Food and Drug Administration (FDA) drug approval at the time.
Despite this success, Gleevec therapy could result in the development of Gleevec-resistant CML in patients. Dr. Sawyers set out to understand the resistance mechanisms. His lab and others identified resistance mutations in BCL-ABL that make Gleevec less effective. Based on these results, scientists developed additional BCR-ABL drugs that inhibit some of the resistance mutations. The most recently approved CML drug, asciminib (Scemblix), was approved in October 2021 and uses a novel mechanism to inhibit the BCR-ABL protein, even if the protein harbors a mutation that makes the disease unresponsive to Gleevec and other BCR-ABL inhibitors. “This is a really nice capstone to the Gleevec story,” said Dr. Sawyers.
Following in His Parents’ Footsteps
Dr. Sawyers’ parents were both doctors in Nashville: His mother was an anesthesiologist, and his father was a surgeon. The young Sawyers excelled in school, particularly in science and math, and he attended Princeton University in New Jersey. For two summers starting after his senior year of high school, he worked as a scrub technician—an assistant who provides the surgeon with sterile equipment during a surgery—at the hospital where his mother was an anesthesiologist. The experience led him to believe that medical school was not likely in his future. Instead, he was drawn to the humanities, majoring in history with a focus on the history of science. During his senior year, he wrote a thesis on the transformation of medical education in China in the 20th century, from training grounded in Western medical traditions to a return to traditional Chinese medicine. Eventually, Sawyers was drawn to medicine and entered medical school at Johns Hopkins in 1981.
Pivoting to Prostate Cancer
Dr. Sawyers’ career has spanned more than three decades. He takes a systematic approach to understanding how certain tumor cells are wired and in identifying the molecules essential for their growth in order to enable drug development. In 2006, Dr. Sawyers’ laboratory moved to Memorial Sloan Kettering Cancer Center, and he became head of the new translational research program that would generate and use genomics data to molecularly understand tumors and develop targeted therapies against them. Driven by his interest in resistance mechanisms and the challenge to find new treatments for solid tumors, Dr. Sawyers’ lab began to study how prostate tumors become resistant to hormone therapy, a commonly used systemic treatment in men with metastatic prostate cancer.
Dr. Sawyers was drawn to prostate cancer in part because it is more common than CML and because of the scientific puzzles the disease presents. In 2004, his lab identified the cause of hormonal therapy resistance: a surge in the expression of androgen receptors that makes therapy ineffective. Together with the UCLA-based biochemistry lab of Michael Jung, PhD, Dr. Sawyers’ laboratory developed a novel anti-androgen therapy, enzalutamide (Xtandi), now approved by the FDA to treat prostate cancer resistant to androgen therapy.

More recently, Dr. Sawyers’ lab has tackled another puzzle—understanding how resistance mechanisms that have emerged to the anti-androgen signaling therapy, including Xtandi, come about. Some patients with relapsed disease have tumors that do not appear to be reliant on the androgen pathway for their growth. These tumors are made up of cells that resemble neuroendocrine cells under the microscope, rather than the typical epithelial cells that make up prostate tumors that do rely on androgens to grow. Studying these distinct prostate tumors, the lab has uncovered a novel way that some of them are able to continue growing, even as they are exposed to prostate cancer therapy. Dr. Sawyers and his lab members found that cells surrounding the prostate tumor can help the tumors become resistant to hormone therapy by secreting higher levels of a specific protein. Other researchers are now working on potential drugs to target the protein, according to Dr. Sawyers.
Dr. Sawyers also continues to analyze the mutations that drive the transformation of prostate cells to prostate cancer. “While prostate cancer therapy targets the androgen pathway, the androgen receptor is not an oncogene itself, it’s not the cause of the transformation of prostate cells,” said Dr. Sawyers. From tumor sequencing, researchers have identified two transcription factors, ERG and FOXA1, both of which, when mutated, appear to be drivers of prostate tumor growth. Interestingly, ERG and FOXA1 mutations are never found in the same prostate tumor—the tumor either has one or the other. “But if you show a pathologist a tumor with either mutation, they can’t tell the difference, suggesting that both of these transcription factors have the same function in the tumor,” Dr. Sawyers explained. In 2019, his lab demonstrated the molecular ways that FOXA1 mutations drive changes in the prostate that lead to prostate cancer. There are few cancer drugs that target transcription factors, but Dr. Sawyers said labs are working on this, and he is hopeful that eventually one will succeed in developing such a drug.
Enabling Collaborative Tumor Genomics
At Memorial Sloan Kettering, Dr. Sawyers was instrumental in centralizing tumor sequencing efforts—building a core sequencing facility, promoting tumor sequencing of patients’ biopsies, and systematically adding the data to an internal research database. As president of the American Association for Cancer Research (AACR) from 2013 to 2014, Dr. Sawyers conceived of a publicly available, large-scale tumor sequencing registry with clinical-grade, matched tumor sequences and clinical information on patients who have and have not yet received therapy for their cancer. Dr. Sawyers helped this vision come to life, bringing together institutions in the U.S., Canada, and Europe to contribute data to the registry. The initiative, called AACR Project GENIE®, now encompasses tumor DNA sequences from over 121,000 patients and more than 136,000 tumors. Dr. Sawyers was the founding chair of the Steering Committee for AACR Project GENIE®.

“Charles is a visionary leader. He recognized the power of leveraging clinical sequencing data at our institutions to benefit the wider cancer research community and conceived of Project GENIE®,” said Philippe Bedard, MD, associate professor of medicine at the University of Toronto in Ontario and the current chair of Project GENIE®. “He is a great listener, able to connect with different perspectives to work towards a shared goal and has played a key role in breaking down barriers and promoting a collaborative culture of data sharing among scientists.”
Leading by Example With Optimism
In 2021, Dr. Sawyers received the AACR Distinguished Public Service Award, presented to individuals whose work exemplifies the AACR’s mission to prevent and cure all cancers through activities that include research, education, collaboration, advocacy, and science policy. He was also awarded the first STAT Biomedical Innovation Award in 2019, given to a top researcher in biomedicine whose work has contributed to defining their field and helping patients. Dr. Sawyers is also a Fellow of the AACR Academy and is currently its second president, serving through 2023.
“Dr. Sawyers is a highly esteemed physician-scientist who has generated an exceptional body of translational and clinical research,” said Margaret Foti, PhD, MD (hc), chief executive officer of the AACR. “His groundbreaking discoveries have provided deep insight into the mechanisms of drug resistance and have led to the development of new molecularly targeted therapies that are benefiting countless patients worldwide.”

In his laboratory, Dr. Sawyers is a unique mentor. “In a noisy world of science, Charles’ approach is always incisive and constructive,” said Rohit Bose, MD PhD, a former clinical and post-doctoral fellow in Dr. Sawyers’ lab at Memorial Sloan Kettering and now an assistant professor and genitourinary medical oncologist at the UCSF Helen Diller Family Comprehensive Cancer Center in San Francisco. “He is so passionate about biomedical research, but equally deft and refined in mentoring trainees to independence. I inwardly smile when I catch myself emulating something he did, or at least trying to emulate him, with my own lab members. It was an absolute pleasure learning from such an amazing scientist and mentor.”
Dr. Sawyers has seen the cancer field progress from having little understanding of cancer’s molecular mechanisms to the genomics era that has brought a sudden explosion and availability of sequencing data, thanks to consortia such as The Cancer Genome Atlas and AACR Project GENIE®. We now know many of the mutations that drive tumor growth and progression.
“The cancer field has evolved tremendously since I began my career,” said Dr. Sawyers. “When I first started working on Gleevec, we were at a stage when we knew only a few of the genes that could cause cancer. For many tumor types, we didn’t know anything. Sequencing came to the rescue, and we generated and analyzed so much data that now we know almost all of the mutations.”
The cancer field is now moving into a different stage of extracting and putting these data pieces together. “There are hundreds of different cancers, and we are still in the process of figuring out how to best treat each one,” Dr. Sawyers said. “There are and will be broad solutions, such as the immune checkpoint inhibitor antibodies, for some of these cancers. There are and will also be individualized solutions for other tumors, like targeting the BCR-ABL gene in CML.”
There are scientists trying to make drugs against targets that 20 years ago we thought couldn’t be targeted.
Dr. Sawyers is optimistic about the cancer field continuing to get a handle on cancer therapy resistance. “Particularly for targeted therapies, we understand the acquired resistance mutations that occur to many molecularly targeted drugs. This knowledge is driving much better next-generation molecular inhibitors. The paradigm that is emerging is that we can anticipate what is going to happen ahead of time and develop targeted agents.”
Even for tumor types for which there are no or few targeted therapies that work, Sawyers is optimistic that researchers will find solutions. “There are scientists trying to make drugs against targets that 20 years ago we thought couldn’t be targeted,” he said. “Cancer is complicated but solvable.”